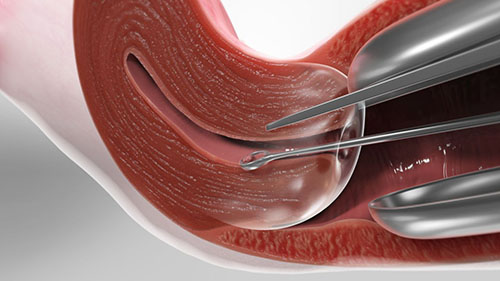
Dilation and curettage (D&C) or sometimes spelled as dilatation and curettage, refers to the dilation (widening/opening) of the cervix and surgical removal of part of the lining of the uterus and/or contents of the uterus by scraping and scooping (curettage). It is a therapeutic gynecological procedure as well as a rarely used method of first trimester abortion.
D&C normally is referred to a procedure involving a curette, also called sharp curettage. However, some sources use the term D&C to refer more generally to any procedure that involves the processes of dilation and removal of uterine contents, which includes the more common suction curettage procedures of manual and electric vacuum aspiration.
Indications
D&Cs are commonly performed for the diagnosis of gynecological conditions leading to 'abnormal uterine bleeding'; to resolve abnormal uterine bleeding (too much, too often or too heavy menstrual flow); to remove the excess uterine lining in women who have conditions such as polycystic ovary syndrome (which cause a prolonged buildup of tissue with no natural period to remove it); to remove tissue in the uterus that may be causing abnormal vaginal bleeding, including postpartum retained placenta; to remove retained tissue (also known as retained POC or retained products of conception) in the case of a missed or incomplete miscarriage; and as a method of abortion that is now uncommon. In contrast, D&C remains 'standard care' for missed and incomplete miscarriage in many countries despite the existence of alternatives currently used for abortions.
Because medical and non-invasive methods of abortion now exist, and because D&C requires heavy sedation or general anesthesia and has higher risks of complication, the procedure has been declining as a method of abortion. The World Health Organization recommends D&C as a method of surgical abortion only when manual vacuum aspiration is unavailable. According to the Centers for Disease Control and Prevention, D&C only accounted for 2.4% of abortions in the United States in the year 2002, down from 23.4% in 1972. Most D&Cs are now carried out for miscarriage management and other indications such as diagnosis.
Alternatives
Hysteroscopy is a valid alternative to D&C for many surgical indications from diagnosis to uterine pathology to removal of fibroids and even retained products of conception. It is less risky due to the ability of the doctor to view inside the uterus during surgery, unlike with blind D&C.
Medical management of miscarriage and medical abortion using drugs such as misoprostol and mifepristone are safe, non-invasive and cheaper alternatives to D&C.
Preparation
Because opening the cervix can be painful, sedatives may be given before the procedure begins. Deep breathing and other relaxation techniques may help ease cramping during cervical dilation.
Aftercare
A woman who has had a D&C performed in a hospital can usually go home the same day or the next day. Many women experience backache and mild cramps after the procedure, and may pass small blood clots for a day or so. Vaginal staining or bleeding may continue for several weeks.
Most women can resume normal activities almost immediately. Patients should avoid sexual intercourse, douching, and tampon use for at least two weeks to prevent infection while the cervix is closing and to allow the endometrium to heal completely.
Nursing Interventions
- Obtain preoperative vital signs of client.
- Conduct health education before the operation on the following topics:
- Signs and symptoms of infection like increasing body temperature, foul smelling discharges from the perineum, moderate to severe abdominal cramps
- Advise that should any sign of infection occurs, it must be reported immediately to the nurse on duty for validation and evaluation
- Good perineal hygiene
- Use of tampons is contraindicated, use perineal pads instead
- No sexual intercourse until vaginal discharge stops
- Coordinate with the OR/DR team to ensure that aseptic technique will be maintained during the entire procedure of D & C.
- Monitor for signs and symptoms of infection inclusive of vital signs and post D & C CBC count.
Risks
The primary risk after the procedure is infection. Signs of infection include:
- fever
- heavy bleeding
- severe cramps
- foul-smelling vaginal discharge
A woman should report any of these symptoms to her doctor, who can treat the infection with antibiotics before it becomes serious.
Dilation and Curettage is a surgical operation, which carries certain risks associated with general anesthesia. Rare complications include puncture of the uterus (which usually heals on its own) or puncture of the bowel or bladder (which requires further surgery to repair).
Normal Results
Results are considered normal if no unusual thickening, growths, or cancers are found. Removal of the uterine lining causes no side effects, and may be beneficial if the lining has thickened so much that it causes heavy periods. The uterine lining soon grows again normally, as part of the menstrual cycle.
Abnormal Results
Some types of uterine thickening, called hyperplasia, are considered abnormal. Simple hyperplasia is a benign condition in which the uterine lining becomes thicker and with more endometrial glands. In complex hyperplasia, another condition where the uterine lining has thickened, the endometrial glands are crowded together. In 80% of cases these conditions will improve, and there is little risk of cancer. Only 1% of simple hyperplasia and 3% of complex hyperplasia will become cancerous.
Atypical hyperplasia is a more serious finding. In this type of endometrial thickening, the cells are abnormal. Twenty-nine percent of women with atypical hyperplasia develop cancer. In fact, in 17% to 25% of women with atypical hyperplasia who have a hysterectomy within one month of diagnosis, a carcinoma is found elsewhere in the endometrium.
Complications
Complications may arise from either the introduction or spreading of infection, adverse reaction to general anesthesia required during the surgery or from instrumentation itself, as the procedure is performed blindly (without the use of any imaging technique such as ultrasound or hysteroscopy).
One risk of sharp curettage is uterine perforation. Although normally no treatment is required for uterine perforation, a laparoscopy may be done to verify that bleeding has stopped on its own. Infection of the uterus or fallopian tubes is also a possible complication, especially if the woman has an untreated sexually transmitted infection.
Another risk is intrauterine adhesions, or Asherman's syndrome. One study found that in women who had one or two sharp curettage procedures for miscarriage, 14-16% developed some adhesions. Women who underwent three sharp curettage procedures for miscarriage had a 32% risk of developing adhesions. The risk of Asherman's syndrome was found to be 30.9% in women who had D&C following a missed miscarriage, and 25% in those who had a D&C 1–4 weeks postpartum. Untreated Asherman's syndrome, especially if severe, also increases the risk of complications in future pregnancies, such as ectopic pregnancy, miscarriage, and abnormal placentation (eg.placenta previa and placenta accreta). According to recent case reports, use of vacuum aspiration can also lead to intrauterine adhesions.
Videos
The video is age-restricted, you may have to watch it from this link.