COVID-19 stand for "Coronavirus Disease 2019", is an infectious disease caused by the SARS-CoV-2 virus. The first documented case emerged in Wuhan, China, back in December 2019. The disease rapidly spread worldwide, resulting into the global COVID-19 pandemic.
Symptoms of COVID-19 may vary, but often include fever, cough, headache, fatigue, breathing difficulties, and loss of smell and taste. These symptoms typically manifest within one to fourteen days post exposure, although about a third of infected individuals remain asymptomatic. Among those exhibiting symptoms, approximately 81% experience mild to moderate symptoms, while 14% develop severe symptoms such as dyspnea, hypoxia, and lung involvement, and 5% develop critical conditions including respiratory failure, shock, or multiorgan dysfunction. Higher risks are linked to age and underlying health conditions like cardiovascular issues, diabetes, chronic respiratory problems, or cancer. However, COVID-19 can infect anyone regardless of age, and may lead to severe illness or fatalities. Elderly individuals face a higher risk of severe symptoms, and some suffer long-term effects known as "long COVID," often with organ damage observed.
On January 30, 2020, COVID-19 was declared a Public Health Emergency of International Concern (PHEIC) with an official death toll of 171. By December 31, 2020, this figure stood at 1,813,188. Yet preliminary estimates suggest the total number of global deaths attributable to the COVID-19 pandemic in 2020 is at least 3 million, representing 1.2 million more deaths than officially reported.[Source]
Signs and Symptoms
Symptoms of COVID-19 varies. Some people may show no signs of the disease but can still spread the disease. Common symptoms include:
Other symptoms include:
- Headaches
- Chills
- Nasal congestion
- Runny nose
- Muscle pain
- Chest pain
- Sore throat
- Diarrhea
- Eye irritation (ie. conjunctivitis)
- Toes swelling or turning purple
- Breathing difficulties
- Rash
- Nausea
- Vomiting
Researchers have recognized three common clusters of symptoms:
- Respiratory symptom cluster with cough, sputum, shortness of breath, and fever.
- Musculoskeletal symptom cluster with muscle pain, joint pain, headache, and fatigue.
- Digestive symptom cluster encompassing abdominal pain, vomiting, and diarrhea.
Loss of taste and smell occurs in up to 88% of symptomatic cases of people without prior ear, nose, or throat disorders.
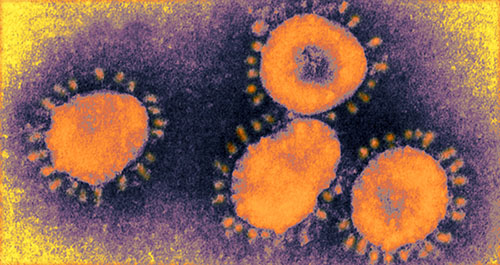
Causative Agent
SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2).
Coronavirus is a family of viruses that can cause illnesses such as the common cold, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS).
A multitude of SARS-CoV-2 variants fall into clades or lineages. The WHO, in collaboration with partners, expert networks, national authorities, institutions and researchers, have established nomenclature systems for naming and tracking SARS-CoV-2 genetic lineages by GISAID, Nextstrain and Pango. The expert group convened by the WHO recommended the labelling of variants using letters of the Greek alphabet, for example, Alpha, Beta, Delta, and Gamma, giving the justification that they will be easier and more practical to discussed by non-scientific audiences. Nextstrain divides the variants into five clades (19A, 19B, 20A, 20B, and 20C), while GISAID divides them into seven (L, O, V, S, G, GH, and GR). The Pango tool groups variants into lineages, with many circulating lineages being classed under the B.1 lineage.
Several notable SARS-CoV-2 variants emerged in 2020, including Cluster 5 from minks and mink farmers in Denmark. Subsequent strict quarantines and mink euthanasia campaigns led to its cessation among humans in Denmark by February 1, 2021.
By December 2021, there are five dominant SARS-CoV-2 variants spreading among global populations: Alpha (B.1.1.7, formerly the UK variant), initially discovered in London and Kent; Beta (B.1.351, formerly the South Africa variant); Gamma (P.1, previously called the Brazil variant); Delta (B.1.617.2, once called the India variant); and Omicron (B.1.1.529), which had spread across 57 countries as of December 7, 2021.
Mode of Transmission
COVID-19 primarily spreads through the inhalation of contaminated air carrying virus-laden droplets, aerosols, and small particles. Infected individuals release these particles while breathing, talking, coughing, sneezing, or singing. Transmission occurs via inhaling infectious particles or contact with eyes, nose, or mouth. Transmission is more probable in close proximity, but it can occur at greater distances indoors. Additionally, the virus can be transmitted from touching contaminated surfaces and subsequently touching facial areas. Individuals can remain contagious for up to 20 days, potentially spreading the virus without exhibiting symptoms.
Virus transmission occurs through respiratory fluid particles, or droplets, expelled from the mouth and nose. There are three types of transmission—"droplet" and "contact," which involves larger droplets, and "airborne," which is linked to smaller droplets. Larger droplets settle quickly and contaminate nearby surfaces, while smaller droplets evaporate faster. These droplets form a nuclei, and remain suspended in the air for a long period of time over extensive distances.
Infectivity can begin four to five days before onset of symptoms. Even pre-symptomatic or asymptomatic individuals can spread the disease. The highest viral load usually occurs around symptom onset, declining within the first week. People with mild to moderate COVID-19 are infectious for about ten days following the onset of symptoms, while severe cases, including immunocompromised individuals, can remain infectious for up to 20 days post-symptom onset.
Infectious particles range from long-lasting aerosols to larger droplets that either briefly stay airborne or settle. Research on COVID-19 has reshaped the traditional understanding of how respiratory viruses are transmitted. Larger droplets of respiratory fluid do not travel far and therefore only pose a localized risk, but can be inhaled or land on mucous membranes on the eyes, nose, or mouth to infect. Aerosols are more concentrated in close proximity, which facilitates easier viral transmission when people are physically close. Airborne transmission can occur at longer distances in poorly ventilated spaces, where small particles can linger for minutes to hours, increasing infection risks.
Incubation Period
It varies depending on the virus variants and the individual immunity.
The incubation period of COVID-19 usually ranges from 2 to 14 days, with an average of 5 to 6 days for earlier strains. Some variants, like Omicron, have a shorter incubation period (3 to 4 days).[Source]
Risk Factors
- Age. Chances of getting seriously sick with COVID-19 go up with age.
- Heart problems
- Long-term kidney disease
- Cancer
- Chronic obstructive pulmonary disease (COPD)
- Diabetes
- Asthma
- Weakened immune system
- Obesity
- Sickle cell disease
- Genetics
Diagnosis
Diagnosing COVID‑19 generally involves symptom assessment and confirmation through tests like reverse transcription polymerase chain reaction (RT-PCR) or similar nucleic acid tests such as transcription-mediated amplification, and reverse transcription loop-mediated isothermal amplification (RT-LAMP) from nasopharyngeal swabs, and examining infected secretions. Additionally, chest CT scans might aid diagnosis in cases with strong clinical suspicion of infection. Serological tests detecting antibodies can indicate past infections.
Viral Testing
The standard methods of testing for presence of SARS-CoV-2 are Nucleic acid tests, primarily RT-PCR, which detects the presence of viral RNA fragments. However, its ability to determine infectivity duration is limited. Samples are usually obtained via nasopharyngeal swabs, nasal swabs, or sputum. Results typically arrive within hours, with WHO offering various testing protocols. Several laboratories and companies have developed serological tests that can detect infection-induced antibodies.
The University of Oxford's CEBM has pointed to mounting evidence that a good proportion of "new" mild cases and individuals re-testing positive post-quarantine or after discharge from hospital might not be infectious, but merely clearing harmless virus particles which their immune system has efficiently dealt with. Efforts are urged to standardize and periodically recalibrate testing. In September 2020, the UK government issued guidelines for procedures to be implemented in laboratories to provide assurance of positive SARS-CoV-2 RNA results during periods of low prevalence, when there is a reduction in the predictive value of positive test results.
Imaging
Chest CT scans, while not recommended for routine screening, can aid diagnosis in suspected cases. Early infection typically shows bilateral multilobar ground-glass opacities with peripheral, asymmetric, and posterior distribution. As the disease progresses, subpleural dominance, crazy paving (lobular septal thickening with variable alveolar filling), and consolidation may appear. Chest radiographs and computed tomography (CT) showing imaging features that include ground-glass opacities without pleural effusions, are characteristic in symptomatic individuals. While imaging can be faster and more sensitive than PCR, it's less specific and might overlap with other infections.
Coding
In late 2019, the WHO introduced emergency ICD-10 disease codes U07.1 for lab-confirmed SARS-CoV-2 deaths, and U07.2 for clinically or epidemiologically diagnosed COVID‑19 deaths without lab-confirmed SARS-CoV-2 infection.
Pathogenesis / Pathophysiology
Coronaviruses are enveloped, positive-sense, single-stranded RNA viruses. They infect a wide variety of host species. They are largely divided into four genera; α, β, γ, and δ based on their genomic structure. α and β coronaviruses infect only mammals. Human coronaviruses such as 229E and NL63 are responsible for common cold and croup and belong to α coronavirus. In contrast, SARS-CoV, Middle East respiratory syndrome coronavirus (MERS-CoV) and SARS-CoV-2 are classified to β coronaviruses.
The life cycle of the virus with the host consists of the following 5 steps: attachment, penetration, biosynthesis, maturation and release. Once viruses bind to host receptors (attachment), they enter host cells through endocytosis or membrane fusion (penetration). Once viral contents are released inside the host cells, viral RNA enters the nucleus for replication. Viral mRNA is used to make viral proteins (biosynthesis). Then, new viral particles are made (maturation) and released. Coronaviruses consist of four structural proteins; Spike (S), membrane (M), envelop (E) and nucleocapsid (N). Spike is composed of a transmembrane trimetric glycoprotein protruding from the viral surface, which determines the diversity of coronaviruses and host tropism. Spike comprises two functional subunits; S1 subunit is responsible for binding to the host cell receptor and S2 subunit is for the fusion of the viral and cellular membranes. Angiotensin converting enzyme 2 (ACE2) was identified as a functional receptor for SARS-CoV. Structural and functional analysis showed that the spike for SARS-CoV-2 also bound to ACE2. ACE2 expression was high in lung, heart, ileum, kidney and bladder. In lung, ACE2 was highly expressed on lung epithelial cells. Whether or not SARS-CoV-2 binds to an additional target needs further investigation. Following the binding of SARS-CoV-2 to the host protein, the spike protein undergoes protease cleavage. A two-step sequential protease cleavage to activate spike protein of SARS-CoV and MERS-CoV was proposed as a model, consisting of cleavage at the S1/S2 cleavage site for priming and a cleavage for activation at the S2 site, a position adjacent to a fusion peptide within the S2 subunit. After the cleavage at the S1/S2 cleavage site, S1 and S2 subunits remain non-covalently bound and the distal S1 subunit contributes to the stabilization of the membrane-anchored S2 subunit at the prefusion state. Subsequent cleavage at the S2 site presumably activates the spike for membrane fusion via irreversible, conformational changes. The coronavirus spike is unusual among viruses because a range of different proteases can cleave and activate it. The characteristics unique to SARS-CoV-2 among coronaviruses is the existence of furin cleavage site ("RPPA" sequence) at the S1/S2 site. The S1/S2 site of SARS-CoV-2 was entirely subjected to cleavage during biosynthesis in a drastic contrast to SARS-CoV spike, which was incorporated into assembly without cleavage. Although the S1/S2 site was also subjected to cleavage by other proteases such as transmembrane protease serine 2 (TMPRSS2) and cathepsin L, the ubiquitous expression of furin likely makes this virus very pathogenic.[Source]
Respiratory tract
After gaining entry into the body, COVID‑19 targets the ciliated epithelium in the nasopharynx and upper airways.
Autopsies conducted on individuals who succumbed to COVID‑19 have revealed widespread damage to the alveoli and the presence of inflammatory infiltrates containing lymphocytes within the lungs.
Nervous system
Loss of smell, a common symptom in COVID‑19, occurs due to the infection of support cells in the olfactory epithelium, leading to subsequent damage to the olfactory neurons. Medical publications have reported the involvement of both the central and peripheral nervous systems in COVID‑19 cases, with many individuals experiencing neurological or mental health issues. Despite the absence of the virus in the central nervous system (CNS) in most COVID-19 patients with neurological problems, low levels of SARS-CoV-2 have been detected in the brains of deceased COVID‑19 patients, but these results still need to be confirmed. Although the virus has been found in the cerebrospinal fluid during autopsies, the exact mechanism of CNS invasion remains unclear, and may first involve invasion of peripheral nerves due to limited ACE2 levels in the brain. Another possible route is the virus entering the bloodstream from the lungs and traversing the blood–brain barrier to gain access to the CNS, possibly facilitated by infected white blood cells.
Studies conducted during the dominance of the Alpha variant suggested a potential link between COVID-19 and brain damage. Subsequent research involving various variants, including Omicron, indicated cell death in the brain across all variants, though the specific cells affected varied. Whether this damage is temporary or permanent remains unknown. Observed individuals infected with COVID-19, even those with mild cases, exhibited an additional 0.2% to 2% loss of brain tissue in regions associated with the sense of smell compared to uninfected individuals. On average, the overall impact on the brain equated to at least one extra year of normal aging, accompanied by lower scores on cognitive tests, with more pronounced effects observed among older individuals.
Gastrointestinal tract
The virus also impacts gastrointestinal organs due to the high expression of ACE2 in the glandular cells of gastric, duodenal, and rectal epithelium, along with its presence in endothelial cells and enterocytes within the small intestine.
Cardiovascular system
The virus can induce both acute myocardial injury and chronic damage to the cardiovascular system. Around 12% of hospitalized infected individuals in Wuhan, China, displayed acute cardiac injury, a figure that rises in severe cases. Elevated rates of cardiovascular symptoms stem from the systemic inflammatory response and immune system disorders during disease progression. Additionally, the presence of ACE2 receptors in the heart, pivotal for heart function, may contribute to acute myocardial injuries, given their high expression in cardiac tissues.
Individuals transferred to intensive care units due to COVID‑19 infections often experience a high incidence of thrombosis and venous thromboembolism, which may correlate with a poorer prognosis. The presence of blood vessel dysfunction and clot formation, indicated by elevated D-dimer levels due to blood clots, plays a significant role in mortality. Clot-related complications such as pulmonary embolisms and brain ischemic events (strokes) have been observed as severe outcomes in COVID‑19 cases. The infection can trigger a series of vasoconstrictive responses in the body, potentially contributing to decreased oxygenation in pneumonia, including pulmonary vasoconstriction. Additionally, tissue samples from deceased individuals associated with COVID‑19, revealed damage to arterioles and capillaries in the brain.
COVID‑19 can lead to significant structural alterations in blood cells, with some changes persisting for months following hospital discharge. The virus' interaction through ACE2-related entry into lymphocytes might contribute to reduced levels of blood lymphocytes.
Kidneys
Complications linked to the kidneys present another frequent cause of death. Early reports indicate that around 30% of hospitalized patients in both China and New York have encountered kidney injury, even among individuals without prior kidney issues.
Immune System
While SARS-CoV-2 primarily targets ACE2-expressing cells in the respiratory tract, severe COVID‑19 cases exhibit signs of widespread systemic hyperinflammation. Clinical laboratory findings showcasing elevated levels of various interleukins (IL‑2, IL‑7, IL‑6), granulocyte-macrophage colony-stimulating factor (GM‑CSF), interferon gamma-induced protein 10 (IP‑10), monocyte chemoattractant protein 1 (MCP1), macrophage inflammatory protein 1‑alpha (MIP‑1‑alpha), and tumor necrosis factor (TNF‑α) indicate cytokine release syndrome (CRS), revealing an underlying immunopathology.
Interferon alpha plays a dual role in COVID-19 pathogenesis. While aiding virus-infected cell elimination, it also boosts ACE-2 expression, potentially aiding SARS-CoV-2 entry and replication. A competition of negative feedback loops via protective effects of interferon alpha, and positive feedback loops via ACE-2 upregulation may influence COVID-19 outcomes.
Moreover, individuals with COVID‑19-related acute respiratory distress syndrome (ARDS) display classical serum biomarkers of CRS, such as elevated C-reactive protein (CRP), lactate dehydrogenase (LDH), D-dimer, and ferritin levels.
Systemic inflammation leads to vasodilation, allowing inflammatory lymphocytic and monocytic infiltration of the lungs and the heart. In particular, pathogenic GM-CSF-secreting T cells were linked to the recruitment of inflammatory IL-6-secreting monocytes and severe lung pathology. Autopsies also reveal lymphocytic infiltrates as part of the disease presentation.
Viral and Host Factors
Various viral and host factors contribute to the virus's pathogenesis. The spike protein (S-protein), comprising S1 and S2 subunits, attaches to the host receptor ACE2. S1 determines the virus's range and tropism through the receptor-binding domain, while S2 facilitates virus-cell membrane fusion using H1 and HR2 heptad repeat regions. Studies highlight the S1 domain's ability to elicit higher IgG and IgA antibody levels, making spike protein expression a focal point in several effective COVID‑19 vaccines.
The M protein facilitates transmembrane nutrient transport and is responsible for viral envelope formation and bud release. On the other hand, the N and E proteins, serving as accessory proteins, impede the host's immune response.
Human angiotensin-converting enzyme 2 (hACE2) serves as the target for the SARS-CoV-2 virus, triggering COVID‑19. Theoretically, medications like angiotensin receptor blockers (ARB) and ACE inhibitors that increase ACE2 expression might elevate COVID‑19 morbidity. While animal studies hint at potential protective effects of ARBs, no clinical trials have confirmed susceptibility or outcomes. Thus, guidelines for hypertensive patients remain unchanged until further data emerges.
The virus's impact on ACE2 cell surfaces leads to leukocytic infiltration, increased blood vessel and alveolar wall permeability, and reduced lung surfactant secretion, primarily causing respiratory symptoms. The aggravation of local inflammation triggers a cytokine storm and eventually lead to systemic inflammatory response syndrome.
Among healthy adults not exposed to SARS-CoV-2, approximately 35% possess CD4+ T cells that recognize the virus' S protein (especially the S2 subunit), and roughly 50% react to other viral proteins, suggesting cross-reactivity from prior common colds caused by other coronaviruses.
It is unknown whether different persons use similar antibody genes in response to COVID‑19.
Prevention
Numerous countries have rolled out COVID-19 vaccines, initiating mass vaccination campaigns alongside preventive measures such as physical distancing (social distancing), quarantine (for those who are infected), indoor ventilation, avoiding crowded places, mask-wearing, hygiene practices, managing potential exposure durations and avoiding face contact with unwashed hands. While ongoing research aims to develop antiviral drugs, current treatment remains primarily supportive, focusing on symptom management, isolation, and experimental interventions.
To curb transmission, staying informed about the disease and its spread is crucial. Infection can be prevented by maintaining a minimum distance of 1 meter, wearing a well-fitted mask, and practicing frequent hand hygiene or using alcohol-based sanitizers. Adhering to vaccination schedules and local guidelines is pivotal.
The virus spreads through tiny liquid particles from an infected person's mouth or nose during activities like coughing, sneezing, speaking, singing, or even breathing. These particles vary from larger droplets to smaller aerosols. Adhering to respiratory etiquette, like coughing into the elbow, and self-isolating when unwell are essential precautions.
Nursing Interventions
Nursing interventions for COVID-19 can be broadly categorized into the following areas:
- Respiratory care: This includes monitoring the patient's respiratory rate, oxygen saturation, and breathing patterns to detect early signs of respiratory distress. Nurses may also provide respiratory support, such as oxygen therapy or nebulizer treatments, and teach patients breathing techniques to help them clear their airways.
- Infection prevention and control: COVID-19 is a highly contagious virus, so it is important to take steps to prevent its spread. Nurses play a key role in implementing infection prevention and control measures, such as wearing personal protective equipment (PPE), hand hygiene, and isolation precautions.
- Symptom management: COVID-19 can cause a variety of symptoms, such as fever, cough, fatigue, muscle aches, and headache. Nurses may provide medications to relieve these symptoms and help patients stay comfortable.
- Education and support: Nurses provide education to patients and their families about COVID-19, including its symptoms, how to prevent its spread, and how to manage the disease at home. Nurses also provide emotional support to patients and their families, who may be anxious or scared about their diagnosis.
In addition to these general interventions, there are also specific nursing interventions for patients with COVID-19 who are critically ill. These interventions may include:
- Mechanical ventilation. Patients with severe respiratory failure may need mechanical ventilation to help them breathe.
- Prone positioning. Prone positioning is a technique that can help improve oxygenation in patients with severe respiratory failure.
- Extracorporeal membrane oxygenation (ECMO). ECMO is a type of life support that can be used to oxygenate the blood outside the body for patients with severe respiratory failure.
Treatment
As of April 2022, while several medications have gained approval in various countries, not all nations have access to these treatments. Patients in high-risk categories experiencing mild to moderate symptoms can opt for nirmatrelvir/ritonavir or remdesivir, both of which decrease the likelihood of severe illness or hospitalization.
Although highly effective vaccines have notably reduced SARS-CoV-2-related mortality, there remains a need for treatment, especially for those awaiting vaccination and the millions of immunocompromised individuals who might not respond well to vaccination. The cornerstone of management of COVID-19 has been supportive care, encompassing symptom relief through medication, fluid therapy, oxygen support, prone positioning when necessary, and medications or devices to aid other affected vital organs.
The majority of COVID-19 cases are mild, and supportive care involves medications like paracetamol or NSAIDs for symptom relief (fever, body aches, cough), adequate fluid intake, rest, and nasal breathing. Emphasizing good personal hygiene and a nutritious diet is also advised. As of April 2020, the US Centers for Disease Control and Prevention (CDC) recommended self-isolation and wearing face masks for those suspecting they carry the virus.
By November 2020, the use of the glucocorticoid dexamethasone was strongly advised for severe cases treated in hospitals with low oxygen levels, aiming to reduce the risk of death. Some severe cases necessitate noninvasive ventilation or admission to intensive care units for mechanical ventilation to support breathing. The use of extracorporeal membrane oxygenation (ECMO) for respiratory failure is being evaluated for its benefits. Systemic hyper-inflammation, known as the cytokine storm, underlies some severe disease courses.
Prognosis
Currently, the prognosis of most patients is good, with only a few patients being reported as critically ill and the mortality rate ranging from 0 to 14.6%. However, the prognosis of the elderly and those with underlying chronic diseases is poor, and the symptoms of children are relatively mild.[Source]
Complications
COVID-19 can cause a range of complications, some of which can be serious or even life-threatening. The severity of complications can vary depending on a person's age, overall health, and the severity of their COVID-19 infection.
Short-term complications
- Pneumonia: This is an inflammation of the lungs that can make it difficult to breathe.
- Acute respiratory distress syndrome (ARDS): This is a serious lung condition that can cause rapid breathing, low blood oxygen levels, and the need for mechanical ventilation.
- Sepsis: This is a life-threatening infection that can cause organ failure.
- Blood clots: COVID-19 can increase the risk of blood clots, which can occur in the legs, lungs, or brain.
- Heart problems: COVID-19 can cause inflammation of the heart muscle (myocarditis) or irregular heartbeats (arrhythmias).
- Kidney problems: COVID-19 can cause kidney failure in some people.
- Neurological problems: COVID-19 can cause a range of neurological problems, including stroke, encephalopathy, and Guillain-Barré syndrome.
Long-term complications
- Long COVID: This is a term used to describe symptoms that persist for weeks or months after a person has recovered from COVID-19. These symptoms can include fatigue, shortness of breath, cognitive problems, and muscle aches and pains.
- Multisystem inflammatory syndrome in children (MIS-C): This is a rare but serious condition that can affect children who have been infected with COVID-19. It can cause symptoms such as fever, rash, abdominal pain, and heart problems.
Other complications
- Mental health problems: COVID-19 can cause or worsen mental health problems, such as anxiety and depression.
- Social isolation: The pandemic has led to increased social isolation, which can have negative effects on physical and mental health.