Multidrug-resistant tuberculosis (MDR-TB) is a type of tuberculosis (TB) that is resistant to at least two of the most powerful TB drugs, isoniazid (INH) and rifampin. MDR-TB is a public health threat that is practically incurable by standard first-line treatment.
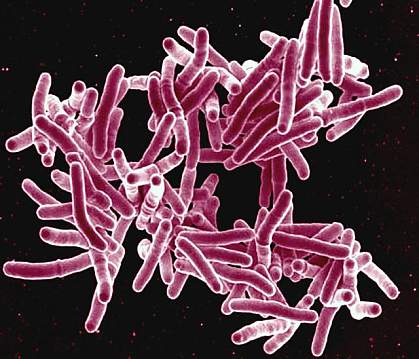
MDR-TB is caused by the bacterium Mycobacterium tuberculosis, which has developed resistance to the first-line drugs. This resistance can occur for a number of reasons, including:
- Inappropriate use of antibiotics: When antibiotics are used incorrectly, the bacteria can develop resistance to them. This can happen when antibiotics are not taken as prescribed, when they are used to treat infections that are not caused by bacteria, or when they are used to treat infections that are not serious.
- Poor quality antibiotics: Antibiotics that are not of high quality may not be effective in killing the bacteria. This can be a problem in developing countries, where access to high-quality antibiotics may be limited.
- Transmission from someone with MDR-TB: MDR-TB can be spread from person to person through the air when an infected person coughs or sneezes.
Signs and Symptoms
The symptoms of Multidrug-resistant tuberculosis are similar to those of TB caused by drug-sensitive bacteria. These symptoms may include:
- Cough
- Fever
- Night sweats
- Weight loss
- Chest pain
- Shortness of breath
Diagnosis
Multidrug-resistant tuberculosis is diagnosed through a combination of tests, including:
- Sputum culture: A sample of sputum is collected from the patient and tested for the presence of the TB bacteria.
- Drug susceptibility testing: The TB bacteria are tested to see if they are resistant to any antibiotics.
Mechanism of drug resistance
The TB bacterium possesses inherent defenses against certain drugs and can develop resistance to drugs through genetic mutations. However, it lacks the capability to transfer resistance genes between organisms via plasmids, a process known as horizontal transfer.
Several mechanisms contribute to drug resistance in TB, including:
- Cell Wall: The cell wall of M. tuberculosis (TB) consists of complex lipid molecules that function as a barrier to prevent drug entry into the cell.
- Drug Modifying and Inactivating Enzymes: The TB genome encodes enzymes (proteins) that can deactivate drug molecules. These enzymes typically modify drug compounds through processes like phosphorylation, acetylation, or adenylation.
- Drug Efflux Systems: TB cells contain molecular systems that actively expel drug molecules from the cell.
- Mutations: Spontaneous mutations in the TB genome can lead to changes in the target proteins of drugs, rendering the bacteria resistant.
One example of such a mutation is found in the rpoB gene, responsible for encoding the beta subunit of the bacterium's RNA polymerase enzyme. In non-resistant TB, rifampin binds to the beta subunit of RNA polymerase, disrupting transcription elongation. However, a mutation in the rpoB gene alters the amino acid sequence and the eventual conformation of the beta subunit. Consequently, rifampin can no longer bind effectively to prevent transcription, leading to drug resistance.
Other mutations can confer resistance to various drugs. For instance, multiple mutations can cause resistance to isoniazid (INH), involving genes like katG, inhA, ahpC, and others. Amino acid replacements in the NADH binding site of InhA seem to result in INH resistance by preventing the inhibition of mycolic acid biosynthesis, an essential component of the bacterium's cell wall. Mutations in the katG gene impair the enzyme catalase peroxidase's ability to convert INH into its biologically active form, rendering INH ineffective and the bacterium resistant.
In certain TB bacteria, the emergence of these mutations can be explained by additional mutations in the DNA recombination, recognition, and repair machinery. These genetic changes increase the overall mutation rate and expedite the accumulation of mutations responsible for drug resistance.
Nursing Interventions
General nursing interventions for MDR-TB include:
- Educating the patient and their family about MDR-TB, including the importance of taking medications as prescribed, the length of treatment, and the risk of side effects.
- Monitoring the patient for side effects of medications and other complications of MDR-TB.
- Providing emotional support to the patient and their family.
Additional nursing interventions for MDR-TB include:
- Ensuring that the patient is placed in airborne isolation precautions to prevent the spread of MDR-TB to others.
- Providing the patient with respiratory support, if needed.
- Monitoring the patient's nutritional status and providing nutritional support, if needed.
- Working with the patient's healthcare team to develop and implement a treatment plan.
Specific nursing interventions for MDR-TB may vary depending on the patient's individual needs. For example, a patient with MDR-TB who is also malnourished may need more intensive nutritional support. A patient with MDR-TB who is experiencing respiratory failure may need mechanical ventilation.
Nurses play a vital role in the care of patients with MDR-TB. By providing comprehensive and compassionate care, nurses can help patients to adhere to their treatment plans, manage their symptoms, and prevent complications.
Treatment
Multidrug-resistant tuberculosis is treated with a combination of antibiotics, including second-line drugs that are not as effective as the first-line drugs. Treatment for MDR-TB typically lasts for 18-24 months.
The treatment for MDR-TB is complex and requires close monitoring by a healthcare provider. Patients with MDR-TB must take their medications as prescribed, even if they start to feel better. Failure to adhere to the treatment regimen can lead to treatment failure and the development of further drug resistance (referred to as Extensively drug-resistant TB or XDR-TB).
It is worth noting that second-line drugs are more expensive than first-line drugs and have more adverse effects.
Prevention
There are a number of things that can be done to prevent the spread of MDR-TB, including:
- Early diagnosis and treatment of TB: Early diagnosis and treatment of TB can help to prevent the development of MDR-TB.
- Education about TB: Education about TB can help people to understand how the disease is spread and how to prevent it.
- Isolation of people with MDR-TB: People with MDR-TB should be isolated to prevent the spread of the disease to others.
Complications
- Treatment failure: This can occur if the MDR-TB bacteria are not completely killed by the antibiotics. Treatment failure can lead to the development of even more drug-resistant TB, which is called extensively drug-resistant TB (XDR-TB).
- Drug toxicity: The antibiotics used to treat MDR-TB can cause serious side effects, such as liver damage, kidney damage, and hearing loss.
- Relapse: This can occur after treatment has been completed, and the MDR-TB bacteria have started to grow again.
- Death: MDR-TB is a serious disease, and it can be fatal, especially if it is not diagnosed and treated early.
In addition to these complications, MDR-TB can also lead to the following:
- Respiratory failure
- Kidney failure
- Heart failure
- Spread of MDR-TB to other people
It is important to note that the complications of Multidrug-resistant tuberculosis can vary depending on the individual's health and the severity of the infection. Some people may experience only mild complications, while others may experience severe complications or even death.