In a recent publication in the journal Nature Reviews Microbiology, researchers summarized over 200 studies that link microbiomes to clinical diagnostic methods and precision therapeutic interventions.
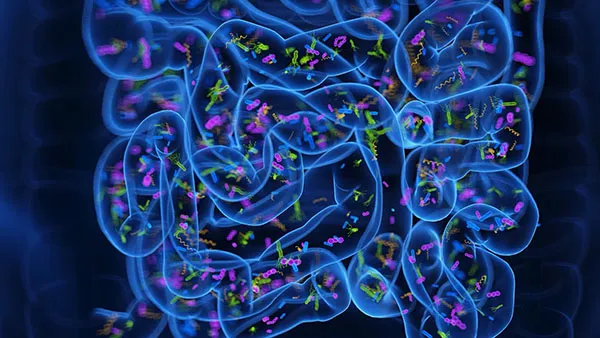
The study explores the gut microbiome, also known as the gut microbiota or gut flora, encompassing all microorganisms residing in the digestive tracts of higher animals.
In contrast to the human host's genome, the gut microbial metagenome displays remarkable variability and adaptability, evolving in response to the host's physiology and environment. These microbial communities are unique to each host, obtained from maternal microbiota and the environment, and are subject to temporal changes.
Individuals vary significantly in their microbiome composition, which can fluctuate within the same individual due to factors like age, location, diurnal rhythms, and various environmental, nutritional, and medicinal exposures.
Mounting evidence underscores the crucial role of gut microbiota in providing nutritional, disease-resistant, and psychological benefits to their host. Disruptions in this ecosystem, termed 'dysbiosis,' have been linked to metabolic, gastrointestinal, neurological, and inflammatory disorders.
Understanding an individual's gut microflora could offer insights into their current health status and facilitate the development of tailored clinical interventions. Current research in personalized treatment primarily focuses on chronic conditions, notably cancer, involving biochemical and genetic phenotyping to guide patient interventions. However, these methods have limitations. For instance, biochemical phenotyping uses standardized methodologies, which can result in binary outcomes with little scope for a nuanced insight of an individual's dynamic health. Similarly, genetic phenotyping fails to account for temporal changes in health or the phenotypic outcomes of gene-environment interactions.
Tailoring treatments based on a patient's microbial community composition overcomes these limitations, ensuring stability within individuals and meeting critical requirements for diagnostic tests.
Advancements in metagenomic sequencing, which analyzes the genetic composition and diversity of the gut microbiome, have identified biomarkers of patients' overall health and specific disease prevalence. These studies have led to the identification of trimethylamine N-oxide (TMAO), a microbiome-modulated metabolite, which plays a role in predicting cardiovascular disease risk, and branched-chain amino acids that helps in predicting type 2 diabetes. Combining metagenomic sequencing with machine learning algorithms has shown promise in distinguishing between glucose intolerance, and typical glucose metabolism with diagnostic accuracy surpassing current diagnostic tools. These findings demonstrate how microbiome analyses with the help of AI can not only replace current diagnostic tools but can significantly reduce clinicians' workload.
Utilizing targeted microbiome interventions to modify disease risks in disease-prone populations complements and optimizes existing prevention methods.
Health behaviors are recognized as pivotal factors in modifying risks associated with various chronic health conditions such as weight, age-related issues, cardiovascular health, and other non-communicable ailments. Numerous studies have outlined optimal behaviors linked to enhancing overall health.
However, recent research indicates that individual responses to behavioral interventions can vary significantly. For instance, while high-intensity physical exercise is beneficial for weight loss, it can lead to blood glucose spikes—a concern for individuals managing type 1 diabetes. Additionally, distinct gut microbiota in individuals process and absorb dietary nutrients differently, impacting their overall health outcomes.
Assessing a patient's gut microbiota through phenotyping enables tailored behavioral and clinical interventions for both common and specific health conditions. Moreover, repeated phenotyping serves as a marker to gauge treatment responsiveness and intervention effectiveness. AI models based on these concepts have exhibited superior performance compared to existing methods in predicting and monitoring how patients respond to clinical interventions.
Emerging research focuses on evaluating the effectiveness of microbial gut supplements and targeted microbiome therapies to prevent or directly tackle communicable diseases. These studies explore diverse approaches, including using microorganisms as drugs to eliminate specific strains of the microbiome, a concept known as 'post-biotic therapy,' utilizing microbial metabolites as drugs.
Beneficial microbes such as pre- and probiotics are either administered directly or encouraged to grow therapeutically, aiming to outcompete or neutralize harmful pathogens. Another method involves addressing dysbiosis, a common condition following antibiotic use that can significantly impact patients' long-term health and immunity. Probiotic supplements are often prescribed alongside or after antibiotic treatments to counter this condition.
The final method involves employing naturally occurring or genetically engineered microbial metabolites as antibiotics. Penicillin, the first known antibiotic, falls in this class.
However, not all patients respond uniformly to these interventions. Identifying those who would benefit the most becomes crucial. In this context, leveraging the individualized microbial profile to serve as an effective 'companion diagnostic' becomes pivotal in tailoring treatments to suit each person's needs.
Despite the promising advantages of utilizing microbiome analyses for disease diagnosis and treatment, this field is still in its early stages. Limited studies have confirmed the safety of these interventions in human subjects.
Ironically, one of the primary strengths of gut microbial interventions—the personalized nature of treatment—poses a significant challenge. Variations among individuals lead to inconsistent data within studies and even less reproducibility across different studies. This inconsistency impedes medical governing bodies from prescribing their use.
Additionally, the novelty of current research drives up costs. Most studies investigating the gut microbiota rely on advanced sequencing methods, which demand expertise and incur expenses beyond the means of researchers and institutions in underdeveloped or developing nations.
Recent research highlights that exposure to microbes, particularly in early childhood, can significantly alter adult microbiome communities and the innate immune system. These findings underscore the necessity for further investigation before personalized clinical approaches can transition from the realm of scientific inquiry to mainstream medical practice.