
Tangier disease is a rare autosomal recessive condition characterized by low levels of high density lipoprotein cholesterol (HDL-C) in the blood, accumulation of cholesterol in many organs of the body, and an increased risk of arteriosclerosis.
Donald Fredrickson was the first to discover Tangier disease. He described this condition in 1961 in a five-year-old boy from Tangier Island who had large, yellow-orange colored tonsils that were engorged with cholesterol. Subsequent tests on this boy and his sister found that they both had virtually no high density lipoprotein cholesterol (HDL-C) in their blood stream. Other symptoms of Tangier disease such as an enlarged spleen and liver, eye abnormalities, and neurological abnormalities were later discovered in others affected with this disease.
It was not until 1999 that the gene for Tangier disease, called the ABCA1 gene, was discovered. This gene is responsible for producing a protein that is involved in the pathway by which HDL removes cholesterol from the cells of the body and transports it to the liver where it is digested and removed from the body.
Cholesterol is transported through the body as part of lipoproteins. Low density lipoproteins (LDL) and high density lipoproteins (HDL) are two of the major cholesterol transporting lipoproteins. Cholesterol attached to LDL (LDL-C) is often called bad cholesterol since it can remain in the blood stream for a long time, and high levels of LDL-C can increase the risk of clogging of the arteries (arteriosclerosis) and heart disease. Cholesterol attached to HDL is often called good cholesterol since it does not stay in the blood stream for a long period of time, and high levels are associated with a low risk of arteriosclerosis.
Research as of 2001 suggests that the ABCA1 protein helps to transport cholesterol found in the cell to the surface of the cell where it joins with a protein called ApoA1 and forms an HDL-C complex. The HDL-C complex transports the cholesterol to the liver where the cholesterol is digested and removed from the body. This process normally prevents an excess accumulation of cholesterol in the cells of the body and can help to protect against arteriosclerosis.
Other names:
Alpha High-Density Lipoprotein Deficiency
Alphalipoproteinemia
Analphalipoproteinemia
Familial Alpha-Lipoprotein Deficiency
Familial High-Density Lipoprotein Deficiency
Familial Hypoalphalipoproteinemia
High density lipoproteindeficiency, type 1 (HDLDT1)
Tangier Disease Neuropathy
Trivia
Tangier disease (TD) is a genetic disorder of cholesterol transport named for the secluded island of Tangier, located off the coast of Virginia. TD was first identified in a five-year-old inhabitant of the island who had characteristic orange tonsils, very low levels of high density lipoprotein (HDL) or 'good cholesterol', and an enlarged liver and spleen.
Signs and Symptoms
The symptoms of Tangier disease are quite variable but the most common symptoms of Tangier disease are enlarged, yellow-colored tonsils, an enlarged spleen, accumulation of cholesterol in the mucous membranes of the intestines, abnormalities in the nervous system (neuropathy), and an increased risk of arteriosclerosis. Less commonly seen symptoms are an enlarged liver, lymph nodes and thymus, and hemolytic anemia. Cholesterol accumulation has been seen in other organs such as the bone marrow, gall bladder, skin, kidneys, heart valves, ureters, testicles, and the cornea of the eye.
The list of signs and symptoms mentioned in various sources for Tangier disease includes the following symptoms listed below:
- Low HDL level
- Mild hypertriglyceridemia
- High fat levels in blood
- Enlarged tonsils
- Orange or yellow tonsils
- Premature atherosclerosis
- Cloudy cornea
- Early-onset cardiovascular disease
Causes
Mutations to chromosome 9q31 lead to a defective ABCA1 transporter. These mutations prevent the ABCA1 protein from effectively transporting cholesterol and phospholipids out of cells for pickup by ApoA1 in the bloodstream. This inability to transport cholesterol out of cells leads to a deficiency of high-density lipoproteins in the circulation, which is a risk factor for coronary artery disease. Additionally, the buildup of cholesterol in cells can be toxic, causing cell death or impaired function. These combined factors lead to the signs and symptoms of Tangier disease.
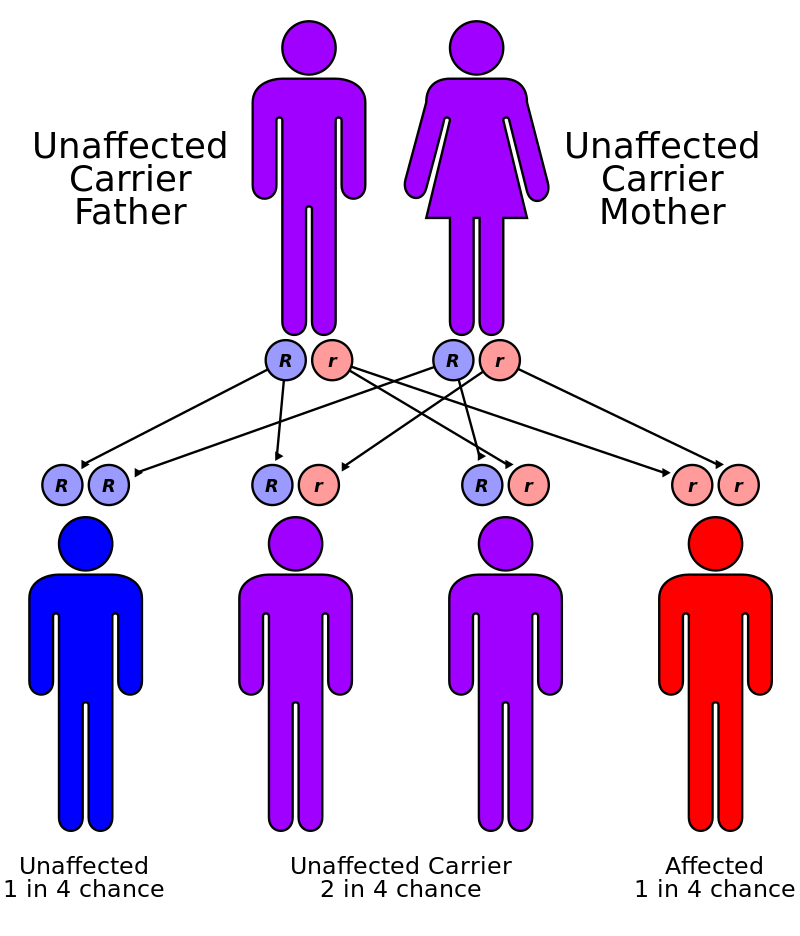
This condition is inherited in an autosomal recessive pattern, which means two copies of the gene in each cell are altered. Most often, the parents of an individual with an autosomal recessive disorder are carriers of one copy of the altered gene but do not show signs and symptoms of the disorder.
Diagnosis
Tangier disease is diagnosed through assessment of clinical symptoms and biochemical testing. A diagnosis of Tangier disease should be considered in anyone with deposits of cholesterol on the cornea, an unexplained enlarged spleen or liver, or neurological abnormalities. Examination of the throat and tonsils and rectal mucous membrane should be performed on those suspected to have Tangier disease. Measurements of the total cholesterol, HDL-C, LDL-C, ApoA1 and triglycerides should also be performed. Patients with Tangier disease have virtually no HDL-C in their bloodstream and ApoA1 levels are reduced to one to three percent of normal. LDL-C levels are also reduced to approximately 40% of normal and triglyceride levels can be mildly elevated.
As of 2001, DNA testing for Tangier disease is not available through clinical laboratories, although DNA testing on a clinical basis should be available in the future. Some laboratories may identify ABCA1 gene changes in patients as part of their research. Prenatal testing is only available if ABCA1 gene changes are identified in the parents.
Pathogenesis / Pathophysiology
TD is caused by mutations in the ABC1 (ATP-binding cassette) gene on chromosome 9q31. ABC1 codes for a protein that helps rid cells of excess cholesterol. This cholesterol is then picked up by HDL particles in the blood and carried to the liver, which processes the cholesterol to be reused in cells throughout the body. Individuals with TD are unable to eliminate cholesterol from cells, leading to its buildup in the tonsils and other organs.
Prevention
No known preventive measures as of this time.
Nursing Interventions
- Monitor for signs and symptoms of coronary artery disease (CAD), stroke, and peripheral artery disease (PAD). This includes monitoring blood pressure, cholesterol levels, and blood sugar levels.
- Provide education on diet and exercise. People with Tangier disease should eat a healthy diet that is low in saturated fat and cholesterol. They should also exercise regularly to help improve their circulation.
- Manage complications of Tangier disease, such as xanthomas, hepatosplenomegaly, and neuropathy. This may involve medication, surgery, or other treatments.
Nursing interventions for specific complications of Tangier disease:
- Xanthomas: Xanthomas are yellowish deposits under the skin that can occur in people with Tangier disease. They are usually harmless, but they can be unsightly. Xanthomas can be treated with medication, surgery, or laser therapy.
- Hepatosplenomegaly: Hepatosplenomegaly is enlargement of the liver and spleen. It is a common complication of Tangier disease. Hepatosplenomegaly can be managed with medications, such as corticosteroids or splenectomy (surgery to remove the spleen).
- Neuropathy: Neuropathy is nerve damage that can occur in people with Tangier disease. It can cause a variety of symptoms, such as numbness, tingling, and pain in the feet and hands. Neuropathy can be managed with medications, such as gabapentin or pregabalin.
Nursing care for patients with Tangier disease should be individualized and based on the patient's specific needs. It is important to work closely with the patient and their family to develop a care plan that addresses the patient's symptoms and helps to prevent complications.
Treatment
There is no treatment for Tangier disease and treatment of decreased HDL-C with medication is usually ineffective. Occasionally organs such as the spleen and tonsils are removed because of extensive accumulation of cholesterol. Arteriosclerosis may be treated through angioplasty or bypass surgery. Angioplasty involves inserting a small, hollow tube called a catheter with a deflated balloon through the groin or arm and into a clogged artery. The balloon is then inflated which enlarges the artery and compresses the blockage. Coronary artery disease can also be treated through bypass surgery, which is performed by taking a blood vessel from another part of the body and constructing an alternate path around the blocked part of the artery.
Complications
- Low density lipoprotein levels low (serum or plasma)
- Lymphadenopathy
- Hypocholesterolemia
- Peripheral neuropathy
- Splenomegaly
- Hepatomegaly
- Corneal opacity
- High density lipoprotein levels low (plasma or serum)
- Autonomic neuropathy, peripheral
- Intermediate density lipoprotein levels raised (plasma or serum)